 Varicose veins are a common condition that affects millions of people worldwide. These twisted, swollen veins can be unsightly and sometimes painful, but understanding the causes and treatment options can help manage the symptoms and prevent complications. In this blog post, we will delve into the world of varicose veins, from what they are to how they can be treated. Reger Vein and Skin Specialist led by Dr. Gregg Reger provides varicose vein treatment to patients in The Woodlands, Spring and Houston TX.
Varicose veins are a common condition that affects millions of people worldwide. These twisted, swollen veins can be unsightly and sometimes painful, but understanding the causes and treatment options can help manage the symptoms and prevent complications. In this blog post, we will delve into the world of varicose veins, from what they are to how they can be treated. Reger Vein and Skin Specialist led by Dr. Gregg Reger provides varicose vein treatment to patients in The Woodlands, Spring and Houston TX.
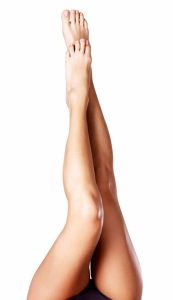
What Exactly Are Varicose Veins?
Varicose veins, characterized by their enlarged, twisted form, emerge predominantly in the legs, presenting a distinctive blue or dark purple hue. This condition stems from an inefficiency in the venous valves, which normally function to propel blood back towards the heart. When these valves become compromised—whether through damage or weakening—blood accumulates within the veins. This stagnation is what leads to the veins’ dilated appearance, a hallmark of varicose veins. The anatomy of the leg, combined with the force of gravity, exacerbates this condition, making the legs the most common site for their development. As blood pools, the veins stretch and twist under the pressure, becoming visibly prominent beneath the skin. This not only affects their appearance but can also lead to discomfort and other symptoms that impact daily life. Understanding the underlying venous anatomy and the role of valve functionality is crucial in grasitating the physiological developments leading to this condition. This insight into their formation underscores the importance of both preventative measures and effective treatment options for those affected by varicose veins.
Unveiling the Causes Behind Varicose Veins
The etiology of varicose veins is multifaceted, involving both genetic and lifestyle factors that compromise venous function and lead to the characteristic bulging and twisting of these veins. A primary factor in the development of varicose veins is heredity. Individuals with a family history of the condition are at a significantly increased risk, suggesting a strong genetic predisposition. Age also plays a crucial role; as the body ages, the veins can lose elasticity, causing the valves to weaken and blood to pool rather than being efficiently returned to the heart.
Hormonal changes, particularly those occurring during pregnancy, can increase venous pressure and the likelihood of developing varicose veins. This is further exacerbated by the additional weight and pressure on the legs during pregnancy, which can hinder venous return. Obesity adds similar strain on the veins, increasing the risk of venous insufficiency and, consequently, varicose veins.
Occupational and lifestyle choices are also influential. Individuals who spend prolonged periods standing or sitting, such as teachers, hairdressers, or office workers, are more susceptible due to decreased circulation and increased pressure in the leg veins. Conversely, engaging in regular physical activity can mitigate some risk by improving overall circulation and venous health. Understanding these contributing factors is essential for both preventing and managing varicose veins, emphasizing the importance of lifestyle modifications alongside medical interventions.
Recognizing the Symptoms of Varicose Veins
Varicose veins manifest through a variety of symptoms that can range from mild discomfort to more pronounced, distressing sensations. Commonly, individuals may experience an uncomfortable feeling of heaviness or fullness in the legs, particularly after prolonged periods of standing or sitting. This sensation often accompanies a throbbing or burning pain in the affected limbs. Swelling in the ankles and feet is another frequent symptom, as is cramping that can disrupt sleep or daily activities.
Beyond physical discomfort, varicose veins can have visible impacts. The skin over and around the veins may itch or become irritated. In more advanced cases, this irritation can lead to eczema or open sores, especially near the ankles. The veins themselves are usually swollen, twisted, and very noticeable beneath the skin, appearing blue or dark purple.
For some, the symptoms may be purely cosmetic, presenting minimal discomfort. However, for others, the symptoms can significantly impair quality of life, indicating the need for careful monitoring and possibly medical intervention to prevent progression and manage discomfort. It’s important for individuals noticing any of these symptoms to consult with a healthcare provider to assess the severity of their condition and explore appropriate treatment options. Recognizing these symptoms early can be crucial in managing varicose veins effectively and minimizing potential complications.
Complications Linked to Untreated Varicose Veins
Neglecting varicose veins can lead to a progression of the condition, resulting in complications that extend beyond cosmetic concerns. One of the more severe consequences includes the formation of blood clots within the affected veins, known medically as thrombophlebitis. This condition not only causes significant pain and swelling but also poses a risk for the clots to travel to other parts of the body, potentially leading to life-threatening situations. Additionally, as blood continues to pool in these twisted veins, the pressure and stagnation may cause the skin around the veins to break down, leading to venous leg ulcers. These ulcers are notoriously difficult to heal and can become chronic sources of discomfort and infection. Furthermore, prolonged venous insufficiency can result in changes to the skin’s texture and color, a condition referred to as lipodermatosclerosis. This can cause the skin to become tight, hard, and discolored, significantly affecting the appearance and health of the legs. Infections are another risk, as the compromised skin and poor circulation associated with varicose veins heighten susceptibility to bacteria, leading to cellulitis, a painful skin infection. These potential complications underline the importance of not dismissing varicose veins as merely an aesthetic issue but recognizing them as a sign of underlying venous disease that warrants medical attention.
Diagnosing Varicose Veins: What to Expect
When seeking a diagnosis for varicose veins, the journey typically begins with a detailed discussion of your medical history and symptoms with a healthcare provider. This conversation aims to identify any genetic predispositions or lifestyle factors that might contribute to your condition. Following this, a physical examination is conducted, focusing on the legs to observe the extent and appearance of the varicose veins. Your doctor might ask you to stand or sit in various positions to evaluate how the veins change and to assess any signs of swelling.
The next step often involves a non-invasive imaging test known as a duplex ultrasound. This diagnostic tool combines traditional ultrasound, which uses sound waves to create images of structures inside your body, with Doppler ultrasound, a technique that can show how blood moves through your veins. Together, these methods provide a comprehensive view of the blood flow in your legs and identify any abnormalities in the vein structure or function. This test is crucial for determining the severity of the varicose veins and crafting a tailored treatment plan.
Throughout this process, your comfort and understanding are paramount. You’ll be encouraged to ask questions and express any concerns, ensuring you’re fully informed and at ease with the diagnostic procedures.
Modern Treatments and Innovations for Varicose Veins
The landscape of varicose vein treatment has seen remarkable advancements, offering patients a range of minimally invasive options that promise effective relief with minimal discomfort and downtime. Compression therapy remains a cornerstone of conservative management, employing specially designed stockings to improve circulation and alleviate symptoms. Sclerotherapy, another popular option, involves the injection of a solution directly into the affected veins, causing them to collapse and fade over time. Laser treatments have also gained traction, utilizing light energy to seal off problematic veins, a process that is both quick and non-invasive. One of the most significant innovations in this field is endovenous ablation therapy, which uses radiofrequency or laser energy to heat and close off varicose veins from the inside. This technique, performed under local anesthesia, allows for an immediate return to daily activities, setting a new standard in vein treatment efficacy and patient convenience. Additionally, emerging therapies and technologies continue to refine our approach to varicose veins, promising even more effective and patient-friendly treatments in the future. Each of these options highlights the commitment to providing patients with safe, effective, and less invasive treatment alternatives.
Preventing Varicose Veins: Tips and Tricks
While completely preventing varicose veins may not be achievable for everyone, especially for those with a strong genetic predisposition, engaging in certain behaviors can significantly lower your risk and may help delay their onset if they’re in your future. Emphasizing regular exercise is key; activities like walking, cycling, and swimming improve leg strength, circulation, and vein health. Keeping your body moving prevents blood from pooling in the leg veins, a primary cause of varicose veins.
Adopting a healthy diet that supports maintaining an optimal weight can also be beneficial. Excess body weight puts additional pressure on your veins, which can exacerbate or lead to the development of varicose veins. Incorporating foods high in dietary fiber can prevent constipation, which, in turn, avoids straining that can increase venous pressure in the legs.
Mind your posture and position throughout the day; if your job requires long periods of standing or sitting, try to change positions regularly or consider using a footrest to elevate your legs when sitting. When standing, shift your weight between legs often.
Finally, elevating your legs above your heart for short periods throughout the day can aid in improving circulation, further helping to prevent the occurrence of varicose veins. By integrating these strategies into your daily routine, you can take proactive steps towards maintaining healthy veins and potentially avoiding the development of varicose veins.
For More Information contact Reger Vein and Skin Specialists in The Woodlands, TX
For more information on procedures and treatments offered by Board Certified Phlebologist Dr. Gregg Reger at Reger Vein and Skin Specialists please call 832-585-0090 or click here to contact our team. Helping patients in Houston, The Woodlands, Springs, Katy and other surrounding areas of Texas.


